NMN & Dry Eye Disease (DED)
2025-01-24 03:18:17
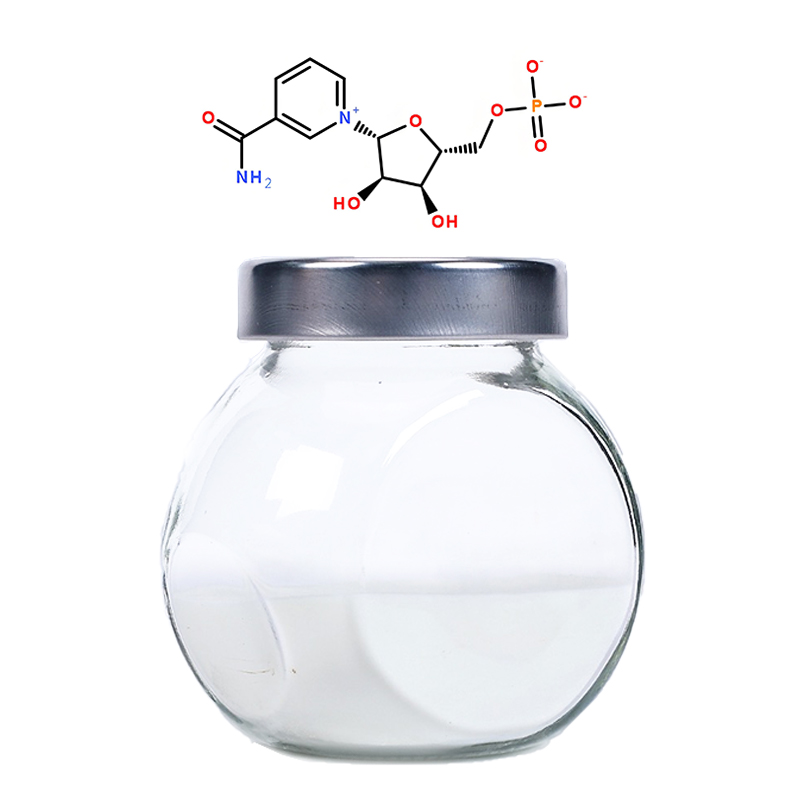
Background: Hyperosmolar stress (HS) is a significant pathological factor in the development of dry eye disease (DED). Nicotinamide mononucleotide (NMN) has demonstrated protective effects against corneal damage; however, its role in HS-induced DED remains unclear.
Methods: An in vitro HS model was established using a hyperosmolar NaCl solution (500 mOsm) and applied to corneal epithelial cells (CECs) and a macrophage cell line, RAW264.7, in a co-culture system. The impact of NMN on NAD+ metabolism and the expression of the HS marker TonEBP in CECs was analyzed. Cell viability, apoptosis, and lactate dehydrogenase (LDH) release were assessed using trypan blue staining, flow cytometry, and LDH assays, respectively. Mitochondrial membrane potential (MMP) was measured with a JC-1 assay kit. Interleukin-17a (IL-17a) expression and secretion were evaluated via RT-PCR, ELISA, and Western blotting. After 24 hours of HS and NMN treatment, the phagocytic capacity and polarization of RAW264.7 cells were observed. Additionally, the expression of the Notch signaling pathway in RAW264.7 cells was analyzed across different groups. The roles of SIRT1 and IL-17a in CEC-mediated regulation of macrophage function were investigated using the SIRT1 inhibitor Ex527 and an anti-IL-17a monoclonal antibody.
Results: NMN intervention increased NAD+ levels in CECs, enhanced cell viability, reduced apoptosis rates, and decreased LDH release. NMN alleviated HS-induced increases in MMP, intracellular reactive oxygen species (ROS) accumulation, and LDH release. In the CEC-macrophage co-culture system, NMN upregulated SIRT1 expression and reduced IL-17a expression and secretion in CECs following HS treatment, thereby diminishing macrophage phagocytic capacity and M1 polarization. Furthermore, NMN-treated CECs inhibited subsequent macrophage activation via the Notch pathway. Studies involving Ex527 and anti-IL-17a antibodies indicated that SIRT1 activation and IL-17a inhibition are crucial mechanisms underlying NMN’s effects.
Conclusion: NMN may serve as a potential corneal protective agent under HS stress by inhibiting IL-17a production and secretion in CECs, thereby modulating macrophage function. The CEC-macrophage co-culture system suggests that the Notch signaling pathway in macrophages contributes to the protective effects of NMN.